Insureous is following the escalating Cornavirus pandemic along with the rest of world.
If you’re wondering, a corona type (2019-nCoV) disease is NOT a pre-existing condition for any carriers. In the unlikely event that you or any of your dependents covered by your policy requires hospitalization the cost will be met by your plan.
In addition, voluntary plans such as Aflac contain benefits should they be diagnosed with COVID-19. If you or your staff has questions about their policies, contact us or call 904-295-8498.
Here are what some of the carriers are covering:
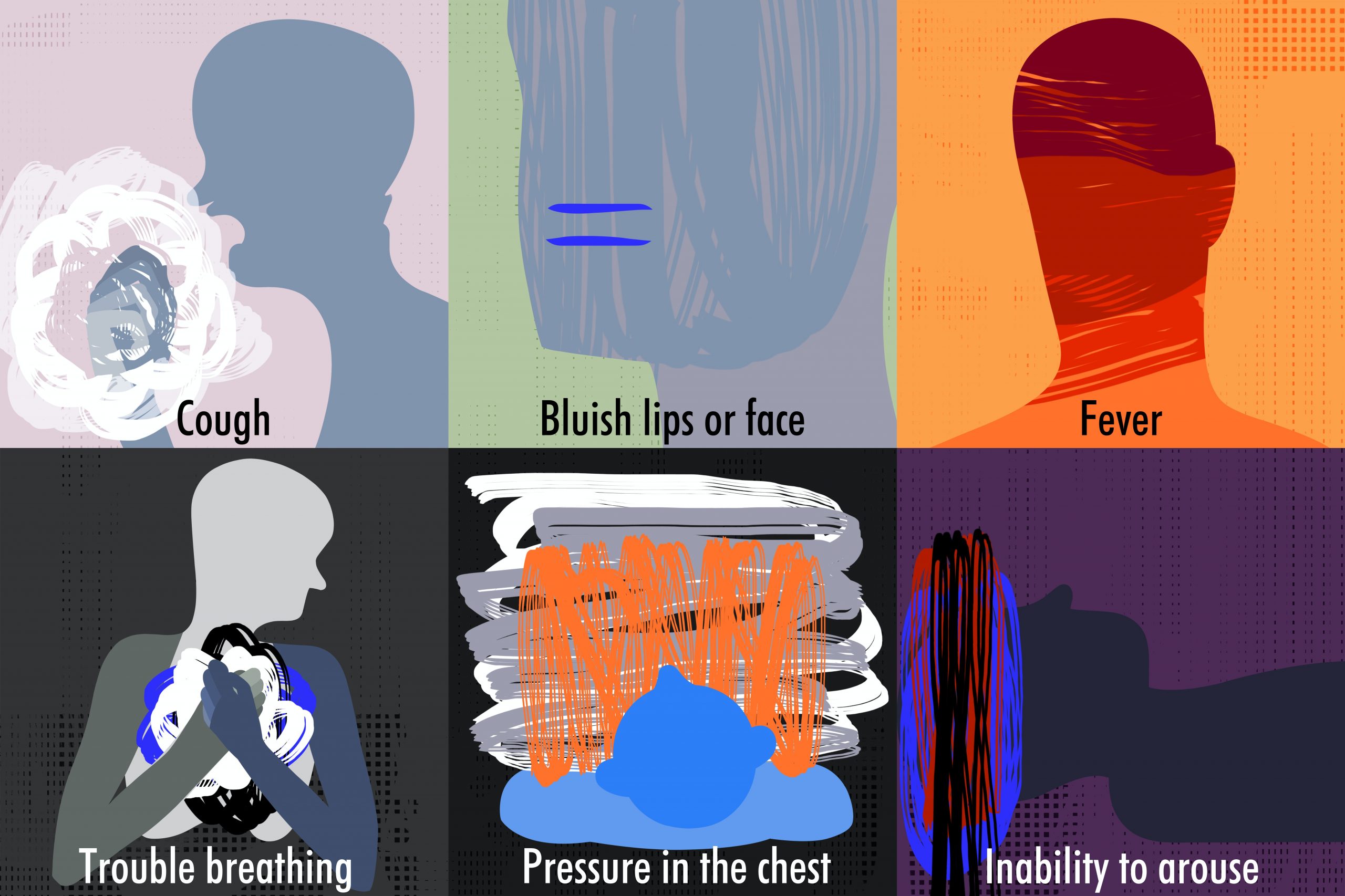
Florida Blue: Florida Blue is making several adjustments to make it easier for members to get tested and treated for COVID-19 and increasing access to other health care services. The company is waiving copays and deductibles related to medical testing for the virus for members who are part of our commercial insurance plans, including Affordable Care Act (ACA)/Individual and Medicare Advantage health plans. Members should consult their health care provider if they are experiencing symptoms linked to the coronavirus, such as mild to severe respiratory symptoms, such as a cough and difficulty breathing, and a fever. If testing is needed, Florida Blue supports the work of providers, the Florida Department of Health and the Centers for Disease Control and Prevention to ensure COVID-19 testing is available. The tests are provided at no cost by state and federal health authorities and may soon be available at other laboratories. Blog
Aetna: Aetna will waive co-pays for all SARS-CoV-2 testing for all insured enrollees, whether the enrollees are in commercial, Medicare or Medicaid plans. Self-insured employers can opt-in. Aetna is also offering zero co-pay telemedicine visits for any reason, and it’s offering its Medicare Advantage virtual evaluation and monitoring visit benefit to all fully insured members. News release
UnitedHealthcare: UnitedHealthcare will waive member cost sharing, including copays, coinsurance and eductibles, for COVID-19 diagnostic testing provided at approved locations in accordance with CDC guidelines for all commercial insured, Medicaid and Medicare members. UnitedHealthcare will also work to support self-insured customers who choose to implement similar actions. Article
Humana: Humana will waive out-of-pocket costs associated with testing for COVID-19 for patients who meet CDC guidelines at approved laboratory locations. This will apply to Humana’s Medicare Advantage, Medicaid and commercial employer-sponsored plans. Self-insured plan sponsors will be able to opt-out of the program at their discretion. The CDC continues to offer free testing for coronavirus. In addition, telemedicine costs waived for all urgent care needs for next 90 days. Article
Medicare: Medicare Part B (Medical Insurance) covers a test to see if you have coronavirus (officially called 2019-novel coronavirus or COVID-19). This test is covered when your doctor or other health care provider orders it, if you got the test on or after February 4, 2020. Article
Insureous are committed to maintaining the service levels that our customers expect. The news around the Coronavirus is changing rapidly. Always refer to the Centers for Disease Control and Prevention, state, and local government guidelines for the most up-to-date information.